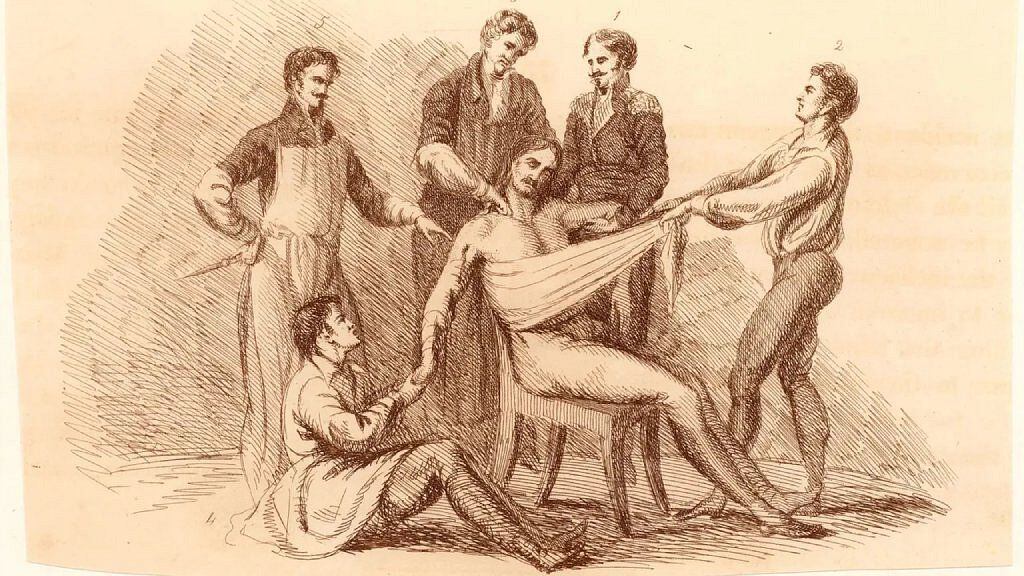
When one day in September 1811 Frances Burney found herself surrounded by 7 men dressed in black and brandishing sharp and sharp objects, she had no choice but to close her eyes, “giving up all observation, all resistance, all interference, and sadly resolved give up completely.”
The celebrated British writer was in Paris, in the hands of an unusually large team of professionals, including two of the leading surgeons of the day, Dominique Jean Larrey, surgeon-in-chief of the imperial army, and Antoine Dubois, Napoleon’s own consulting surgeon.
LOOK: The billionaire trans woman who bought Miss Universe at a time when the contest seeks to be more diverse
Breast cancer had forced her to undergo a harrowing experience.
“Hopeless and desperate” she gave in to the inevitable, she would later tell her sister Esther in a letter that marked “‘A Tale from Paris of a Terrible Operation,” one of the first first-hand descriptions of a mastectomy.
And one of the few that describe in detail the tremendous torment of those who underwent surgery before anesthesia was used.
He knew he was going to “suffer a lot,” as Dubois had warned him, but he had to hang on, “defying a terror beyond description, and the most excruciating pain”.
“However, when the terrible steel plunged into his chest, cutting the veins, the arteries, the flesh, the nerves” of his entrails, “a scream that lasted without interruption during the entire time of the incision (… ) so unbearable was the agony (…) I felt the knife against my sternum, scraping it!”.
Burney’s testimony provides insight into the physical and psychological pain experienced by surgical patients.
And the consequences were not only felt in the body but also in the mind.
“Not for days, not for weeks, but for months I was unable to speak of this terrible affair without almost reliving it!” Burney wrote.
Faced with the prospect of having body parts cut off while in their five senses, patients endured any ailment, to the brink of death, knowing that the pain of relieving it would be worse.
Surgeons, too, had times of such profound distress that, even for the most skilled with the scalpel, operations were a last resort.
Burney says that Dr. Larrey “had tears in his eyes” as he watched the procedure, and that the only time he spoke was to tell them how sorry he was for them, sensing their concern at seeing her suffer so much.
Given so much horror, it’s no wonder that attempts to alleviate pain by producing unconsciousness are almost as old as civilization.
Many were harmless and ineffective while others were downright dangerous.
A toast and various potions
The ingestion of ethanol to induce a kind of detachment from pain was one of the most common practices.
They got the patients drunk until it wasn’t so much that it didn’t hurt but that they didn’t care so much that it hurt.
Alcohol often also served as a solvent in sedative potions, which healers and mystics around the world made from plants that could alter the mind.
One of the oldest examples is the mafeisana mixture of herbal extracts created by the 2nd-century Chinese surgeon Hua Tuo, who, according to “The Book of Later Han,” was the first doctor to perform surgery under anesthesia1,600 years before the practice was adopted in Europe.
The exact recipe has been lost, but the legendary sedative is believed to have contained cannabis or blue flower wolfsbane (Aconitum napellus), a poisonous plant that can be lethal.
This characteristic is shared by some of the ingredients of other sedative potions, such as the beautifully named Belladonna, one of the most toxic plants in the northern hemisphere that, however, was used for centuries in medicinal treatments, or hemlockthat official poison of ancient Greece that killed Socrates.
The latter was one of the ingredients of the English sedative “dwale“, which also contained…
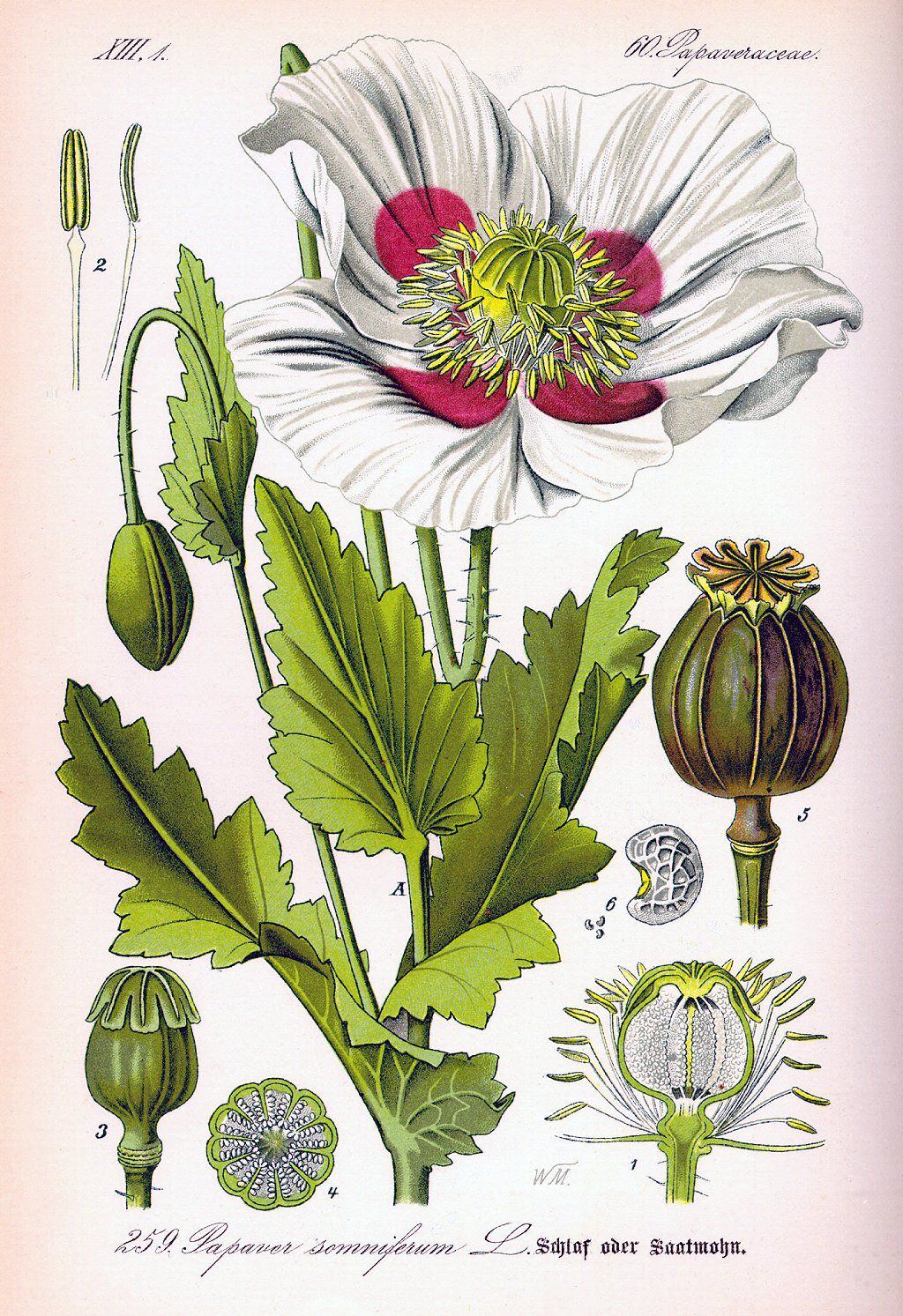
The dwale it is an example of the potions that began to be standardized in the Middle Ages around that particular group of plants.
In the 15th century, a mixture of opium, mandrake and henbane was the preferred sedative for surgical procedures such as amputation, and ever since until the 19th century sedatives changed very little.
However, concoctions were not the only method practiced in pursuit of unconsciousness.
Blows, pressures and mesmerism
If taking potions that, in inexperienced hands, could poison the patient was not very advisable, allowing them to hit you a heavy blow to the head It wasn’t the most attractive option either, but one that, when all else failed or was unavailable, was resorted to to knock out those who needed surgery.
It was a merciful measure, but its consequences could be, among others, head trauma.
Another technique was to apply nerve pressureto cause numbness in the extremities, or neck arteries.

The ancient Greeks called them “carotids,” a name derived from the Greek for stupor or daze, perhaps indicating that it was known ever since that compressing them would cause unconsciousness.
Although the first method was used in 1784 by a British surgeon named John Hunter to amputate a limb and, according to the Royal College of Anaesthetists in the United Kingdom, the amputee felt no pain, the second was not very common… with good reason: the Obstruction of blood flow to the brain put the patient’s life at risk.
Less dangerous was hypnotismintroduced as “animal magnetism” or “mesmerism” in the latter part of the 18th century, which could be effective but only in susceptible individuals.
Speed
Against this background, the best you could hope for was to be in the hands of surgeons like Robert Liston, whose operations at University College Hospital in London in the early 1840s were notorious for their speed, intensity, and success.
Not only was the chance of dying from a Liston amputation 1 in 6, much better than the average Victorian surgeon, but from the first cut until the amputated limb fell into a box of sawdust only 25 seconds passed.

No painkillers available, the skill of surgeons like him shortened that almost unimaginably horrible trauma of surgery.
But that also limited the variety of possible procedures.
More complicated operations required anesthesia, not only to prevent pain but, in some parts of the body, to relax muscles and access organs.
Finally!
Finally, in the middle of the 19th century, the first agent that was successfully demonstrated in public appeared: diethyl ether.
It had originally been synthesized (by the action of sulfuric acid on ethanol) in the 13th century and, although there are early reports of it producing both pain relief and loss of consciousness, such observations were not applied clinically for 600 years.
Chloroform also entered the scene, and the two compounds gave surgeons more time to operate, and therefore to do it more meticulously.
However, in the 1850s there were heated debates about the risks and benefits of anesthesia.
There were questions about whether pain was necessary for surgical success.
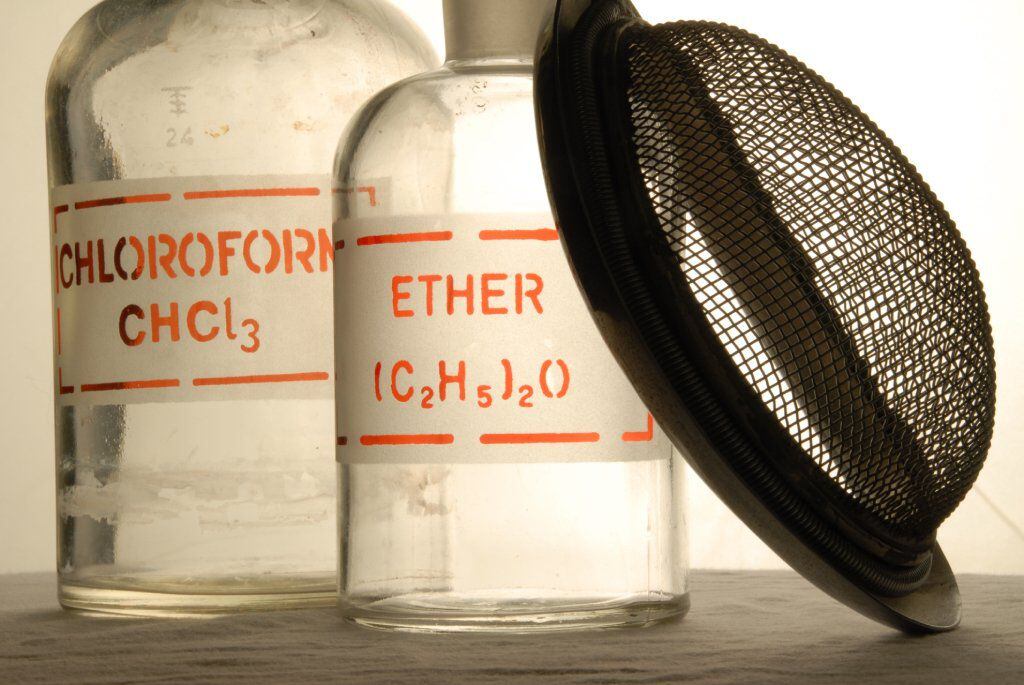
During the Crimean War (1853-1856), the British Army’s chief medicine officer specifically prohibited the use of chloroform in battlefield surgery.
A military surgeon commented that he preferred to listen to “the loud screams” of the soldiers as they went through the operating room. It was a sign, he said, that they were fighting for survival.
“Pain was considered a vital function, since they thought it was like a stimulant for the body to withstand the stress of the operationStephanie Snow, a historian of medicine at the University of Manchester and author of books on the history of anaesthesia, explained to the BBC.
By 1860, however, anesthesia was in common use.
Patients were less likely to refuse surgery, and surgeons were able to take more time with procedures and try new, more sophisticated operations.
In the early 20th century, the first cocaine-based local anesthetics were used, and anesthesiologists began to emerge as a separate profession.
But ether and chloroform, sometimes used in combination, remained the only general anesthetics (although chloroform fell out of use in the 1930s).
It took a world war to develop the drugs and gases used today in operating rooms, which owe their existence to the development of nuclear weapons.
“Nuclear bombs needed uranium hexafluoride and the sudden advance during World War II in fluorination chemistry made it possible to produce highly effective, non-flammable and safer anesthetics,” William Harrop-Griffiths, chairman of the Board, told the BBC. of Research and Clinical Quality of the Royal College of Anesthesiologists of the United Kingdom.
“From something that killed tens of thousands, came drugs that saved hundreds of thousands”.
Source: Elcomercio
I, Ronald Payne, am a journalist and author who dedicated his life to telling the stories that need to be said. I have over 7 years of experience as a reporter and editor, covering everything from politics to business to crime.

:quality(75)/cloudfront-us-east-1.images.arcpublishing.com/elcomercio/URQFIAHEEJCAHCFWPLDSSLYFDY.webp)

:quality(75)/cloudfront-us-east-1.images.arcpublishing.com/elcomercio/QVDFAEXN4RE2JFU5XAD3XBFUOA.jpg)
:quality(75)/cloudfront-us-east-1.images.arcpublishing.com/elcomercio/JGF25CLEPJDGFCOV7R5M6TTNPQ.jpg)
:quality(75)/cloudfront-us-east-1.images.arcpublishing.com/elcomercio/NTCWIM4TFRHULEHO63AN3LQX6E.jpeg)
:quality(75)/cloudfront-us-east-1.images.arcpublishing.com/elcomercio/HC4XATKIGBAH5G47Y5CJNTIJOU.jpg)
